Medicaid And The Dependencies Between States In The United State
February 22 2024
By Isabella Baxter
A window of opportunity has emerged for states to modify Medicaid policies following the enactment of the legislation known as the "Patient Protection and Affordable Care Act" (ACA) and a ruling from the Supreme Court holding that the federal government cannot force states to expand Medicaid. States now have the choice to make Medicaid expansion decisions.
While the available research on Medicaid expansion suggests that political considerations influence state decisions about Medicaid expansion, there is a dearth of thorough assessments in the area of Medicaid policy regarding the primary variables influencing these decisions. This article will examine how state-level policies are decided upon and how pertinent state factors affect Medicaid expansion (1).
The Medicaid expansion made possible by the Affordable Care Act, better known as the ACA, extended coverage to almost every adult with earnings up to 138% of the poverty level set by the government ($20,783 for an individual in 2024). It also gave states a boosted federal matching rate (FMAP) for the growth of their populations.
As of right now, 10 states are yet to implement the expansion, while 41 states (including Washington, DC) have. The current situation of each state is dependent on KFF tracking and evaluation of state expansion activity (2).
A map illustrating the state's position concerning the Medicaid Expansion Decision (3).
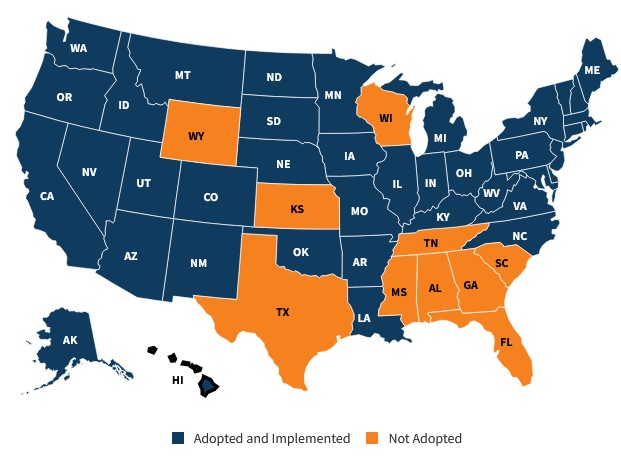
As of January 2022, states in the United States that had expanded Medicaid under the Affordable Care Act include Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, District of Columbia, Hawaii, Illinois, Indiana, Iowa, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Montana, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Dakota, Ohio, Oregon, Pennsylvania, Rhode Island, Vermont, Virginia, Washington, and West Virginia. Please note that Medicaid expansion status may change, and it's advisable to refer to current sources for the latest information (6).
Alabama
Since the start of the Marketplace opening enrollment Period and associated Medicaid program modifications in October 2013, Alabama has signed up 1,123,313 people in Medicaid and CHIP, representing a net gain of 40.56%. This data is as of October 2023. Alabama has implemented several of the targeted registration tactics described in CMS's May 17, 2013, guidelines, which aim to make Medicaid and CHIP enrollment easier (4).
Alaska
As of October 2023, Medicaid and CHIP enrollment in Alaska stands at 211,981 individuals, reflecting a substantial growth of 73.28% since the initial Marketplace Open Enrollment Period and associated Medicaid program modifications in October 2013. Alaska has embraced specific enrollment strategies, as per CMS guidance issued on May 17, 2013, aimed at streamlining the enrollment process for Medicaid and CHIP (5).
Arkansas
In December 2021, the Centers for Medicare & Medicaid Services (CMS) approved Arkansas' Section 1115 waiver proposal, aiming to replace the existing Medicaid expansion initiative, Arkansas Works, with the Arkansas Health and Opportunity for Me (ARHOME) program. Notably, ARHOME, in its approved form, does not incorporate work requirements and has phased out premium obligations for the expansion population, distinguishing it from Arkansas Works. Subsequently, in June 2023, the state submitted a request to modify ARHOME, seeking the flexibility to reassign certain Qualified Health Plan (QHP) enrollees who do not engage in workforce "engagement" activities to receive fee-for-service coverage (7).
California
As of October 2023, California has achieved a noteworthy milestone in healthcare coverage, enrolling a total of 14,008,964 individuals in both Medicaid and CHIP. This remarkable figure signifies a substantial growth of 80.64% since the initiation of the Marketplace Open Enrollment Period and the subsequent adjustments made to the Medicaid program back in October 2013.
California's success in expanding Medicaid and CHIP can be attributed to the deliberate adoption of targeted enrollment strategies. These strategies, outlined in guidance issued by the Centers for Medicare & Medicaid Services (CMS) on May 17, 2013, have played a pivotal role in facilitating and streamlining the enrollment process for individuals seeking Medicaid and CHIP benefits. The state's commitment to implementing these specific strategies reflects a proactive approach to addressing the healthcare needs of its population (8).
Florida
As of October 2023, Florida has enrolled 4,234,627 individuals in Medicaid and CHIP, reflecting a commendable 14.59% increase since the initial Marketplace Open Enrollment Period and related Medicaid program changes in October 2013.
This achievement is attributed to Florida's adoption of targeted enrollment strategies outlined by CMS on May 17, 2013, designed to streamline and facilitate Medicaid and CHIP enrollment. Florida's commitment to these strategies demonstrates a proactive approach to addressing healthcare needs, contributing to increased accessibility and efficiency in healthcare coverage for its diverse population.
Michigan
As of October 2023, Michigan has successfully enrolled 2,904,023 individuals in Medicaid and CHIP, marking a significant 51.88% increase since the inaugural Marketplace Open Enrollment Period and associated Medicaid program adjustments in October 2013.
Michigan's accomplishment in expanding Medicaid and CHIP can be attributed to the strategic implementation of targeted enrollment strategies recommended by the Centers for Medicare & Medicaid Services (CMS) in their guidance issued on May 17, 2013. These strategies play a vital role in simplifying and enhancing the enrollment process for individuals seeking Medicaid and CHIP benefits (4).
In Conclusion
Several U.S. states, including Alaska, California, and Florida, have made significant strides in Medicaid and CHIP enrollment. In Alaska, enrollment has surged by 73.28%, with the state adopting targeted strategies recommended by CMS.
California has witnessed an impressive 80.64% increase, attributing its success to similar CMS-endorsed strategies. Florida, with a 14.59% rise, showcases proactive efforts in healthcare coverage by embracing CMS-recommended enrollment strategies.
Michigan, boasting a 51.88% surge, underscores its commitment to accessible healthcare through the strategic implementation of CMS guidelines.
These states collectively demonstrate effective policy implementation and commitment to improving healthcare access for their diverse populations.
References:
1. https://web.archive.org/web/20200318164214id_/https://digitalcommons.odu.edu/cgi/viewcontent.cgi?article=1003&context=publicservice_etds
2. https://www.kff.org/affordable-care-act/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/#:~:text=To%20date%2C%2041%20states%20(including,analysis%20of%20state%20expansion%20activity.
3. https://www.kff.org/affordable-care-act/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/
4. https://www.medicaid.gov/state-overviews/stateprofile.html?state=michigan
5. https://files.kff.org/attachment/fact-sheet-medicaid-state-AZ
6. https://www.kff.org/statedata/
7. https://www.statista.com/statistics/245400/total-medicaid-spending-in-the-us-by-state/
8. https://www.healthforcalifornia.com/covered-california/health-insurance-companies/medi-cal/medicaid-by-state
Post URL: https://dentistsmedicaid.com/blog/10,Medicaid-And-The-Dependencies-Between-States-In-The-United-State/

|
Written by Isabella Baxter Expert in the medical industry. Writer | Blogger | Dreamer. |